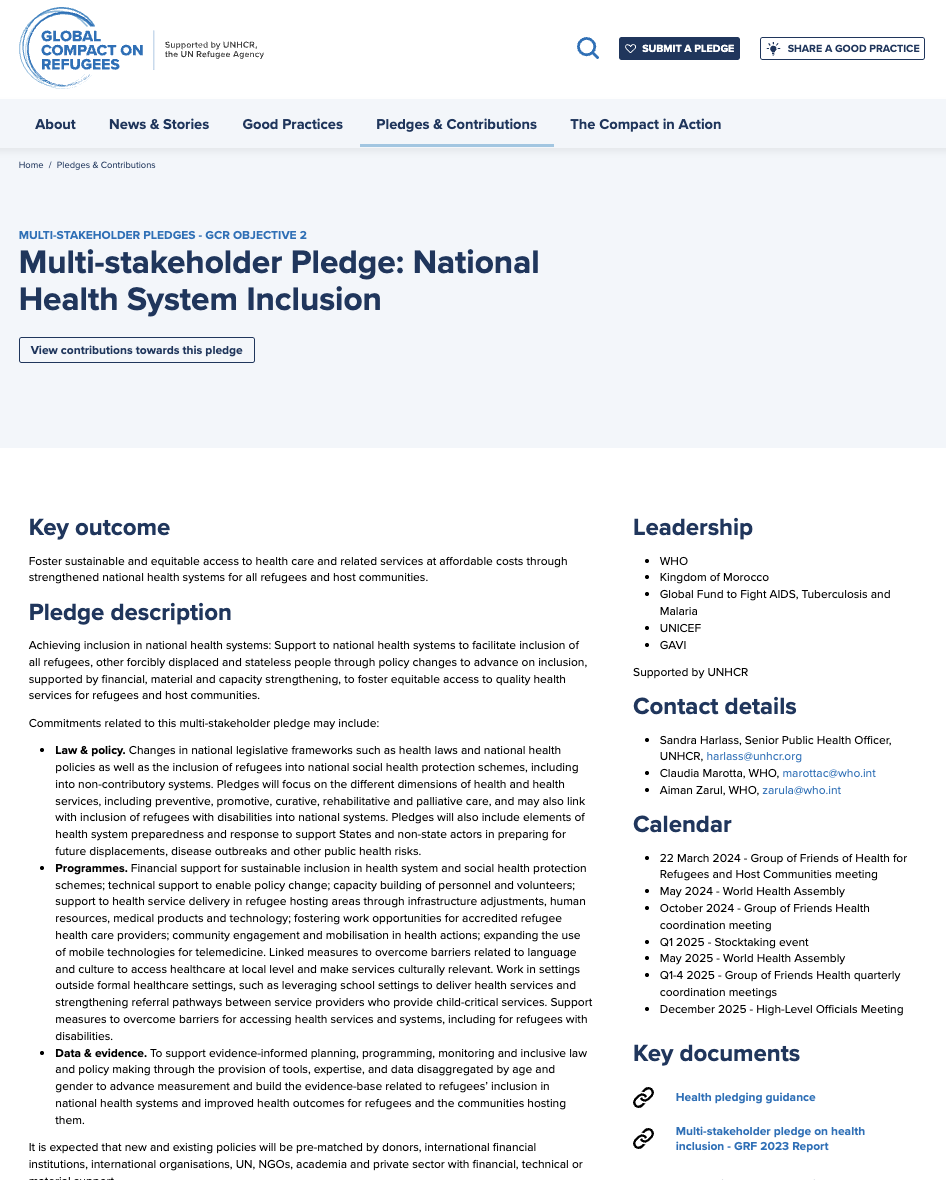
Multi-Stakeholder Pledge: National Health System Inclusion
Author(s)
Abstract
Key Outcome
Foster sustainable and equitable access to health care and related services at affordable costs through strengthened national health systems for all refugees and host communities.
Pledge Description
Achieving inclusion in national health systems: Support to national health systems to facilitate inclusion of all refugees, other forcibly displaced and stateless people through policy changes to advance on inclusion, supported by financial, material and capacity strengthening, to foster equitable access to quality health services for refugees and host communities.
Commitments related to this multi-stakeholder pledge may include:
- Law & policy. Changes in national legislative frameworks such as health laws and national health policies as well as the inclusion of refugees into national social health protection schemes, including into non-contributory systems. Pledges will focus on the different dimensions of health and health services, including preventive, promotive, curative, rehabilitative and palliative care, and may also link with inclusion of refugees with disabilities into national systems. Pledges will also include elements of health system preparedness and response to support States and non-state actors in preparing for future displacements, disease outbreaks and other public health risks.
- Programmes. Financial support for sustainable inclusion in health system and social health protection schemes; technical support to enable policy change; capacity building of personnel and volunteers; support to health service delivery in refugee hosting areas through infrastructure adjustments, human resources, medical products and technology; fostering work opportunities for accredited refugee health care providers; community engagement and mobilisation in health actions; expanding the use of mobile technologies for telemedicine. Linked measures to overcome barriers related to language and culture to access healthcare at local level and make services culturally relevant. Work in settings outside formal healthcare settings, such as leveraging school settings to deliver health services and strengthening referral pathways between service providers who provide child-critical services. Support measures to overcome barriers for accessing health services and systems, including for refugees with disabilities.
- Data & evidence. To support evidence-informed planning, programming, monitoring and inclusive law and policy making through the provision of tools, expertise, and data disaggregated by age and gender to advance measurement and build the evidence-base related to refugees’ inclusion in national health systems and improved health outcomes for refugees and the communities hosting them.
It is expected that new and existing policies will be pre-matched by donors, international financial institutions, international organisations, UN, NGOs, academia and private sector with financial, technical or material support.
